My Opinion About Asthma Severity, Staging, and Control
Prior to the launch of this website, Health Union conducted a survey of asthmatics, many of whom said they had no idea what stage their asthma was in when they were diagnosed. I think this makes sense, because the emphasis among asthma experts has moved away from asthma staging and toward asthma control. Allow me to explain.
What is asthma severity?
It is now understood that all asthmatics have some degree of underlying airway inflammation making their airways hypersensitive, or twitchy, when exposed to asthma triggers. The degree of inflammation determines how twitchy airways are. Asthma severity essentially determines how twitchy your airways are when you are exposed to your asthma triggers.
How is asthma severity determined?
There is no surefire test to measure how “twitchy” your airways are, so asthma severity is based on your perception of the impact of asthma on the quality of your life.
- Intensity of symptoms. How bad are your symptoms when they occur?
- Impairment of physical activities. Do your symptoms stop you from performing your normal activities during the course of a typical day? Do they impact your work? Do they impact your ability to function at school?
- Frequency of symptoms. How often do your asthma symptoms occur? How long are intervals between attacks?
- Responsiveness to treatment. How does your asthma respond to the medicine you take to treat it?1
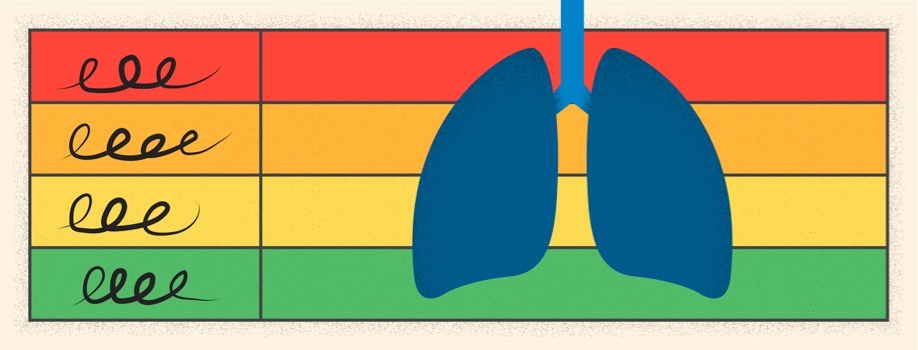
What are the stages of asthma, and why are they important?
These are classifications or levels that determine how severe your asthma is. The idea is that determining what stage of asthma you have should help your doctors determine how aggressive your asthma treatment regimen needs to be in order to obtain ideal control of your asthma. Here are the stages.
- Mild Intermittent Asthma. Your asthma symptoms are mild, easy to control with asthma rescue medicine like 2-3 puffs of an albuterol inhaler, and occur less than 2-3 times in any two week period. Routine use of asthma controller medicines are usually not needed.
- Mild Persistent Asthma. Your asthma symptoms are mild, easy to control with asthma rescue medicine, and may occur more frequently than 2-3 times in a two week period. Routine use of one asthma controller medicine, such as Flovent or Pulmicort, is all that is needed to control your asthma.
- Moderate Persistent Asthma. Your asthma symptoms seem to always be there, and they do not always respond well to rescue medicine. At a minimum, routine use of one asthma controller medicine will control your asthma. However, two asthma controller medicines may be needed, and these are combined in combination inhalers like Advair, Symbicort, Dulera, and Breo.
- Severe Persistent Asthma. Your asthma symptoms seem to always be present, and they do not always respond well to rescue medicine. You will more than likely require routine use of combination inhalers, and require occasional boosts of systemic corticosteroids. An aggressive treatment regimen involving less conventional asthma medicine, like theophyline and Spiriva, may also be required to obtain good asthma control. 2
What is asthma control?
Prior to the late 1980s, the emphasis of asthma treatment programs was to only treat acute (it’s happening now) asthma symptoms. This was accomplished with medicines like asthma rescue medicine and inhaled corticosteroids at home, or epinephrine and systemic steroids at the doctor’s office or hospital. Since then, the goal of asthma treatment programs has shifted to preventing asthma attacks from ever occurring, or at least to making them less severe and easier to control when they do occur. For most asthmatics, this requires taking one or more asthma controller medicines every day.
Why is staging out and controlling in?
First, asthma severity is how bad your asthma is when you are not on any asthma medicine, or before you begin an asthma treatment regimen. Like me, most asthmatics were already on asthma controller medicine prior to meeting their current doctors, and it would not be prudent to take them off their medicine to see how severe it is.
Second, it takes up to 2-3 weeks for asthma controller medicine to get into your system and start working, so it’s not logical to delay beginning a treatment regimen.
Third, it doesn’t matter what stage of asthma you are in, because asthma is asthma. No matter what stage of asthma you are in, the goal is the same: work with your asthma doctor to obtain ideal asthma control. For some it may be as simple as avoiding triggers, although many will require one or more asthma medicines.
I have never had a doctor discuss asthma staging with me.
All that has ever been discussed is that I have asthma. What my doctor says to me each time I see him is, “How are you doing?” If I say, “Good!”, my treatment program stays the same. If I say, “Not good!”, then we tweak something, or try something new. Basically, what we discuss is asthma control, because that’s all that matters.
What stage of asthma do I think I have?
There was a doctor a few years back who wanted me to participate in an asthma research program who was convinced, based on the material I offered her, that I had severe asthma. Based on the definitions offered above, my wife agrees with her, and makes sure any new doctor who sees me is made aware of this fact. I hate when she does that, but it’s probably for the best. I’m usually good for downplaying it, and that’s probably not good either.
So, what do you discuss with your doctor? Do you know what stage of asthma you are in? Let us know in the comments below.
Join the conversation