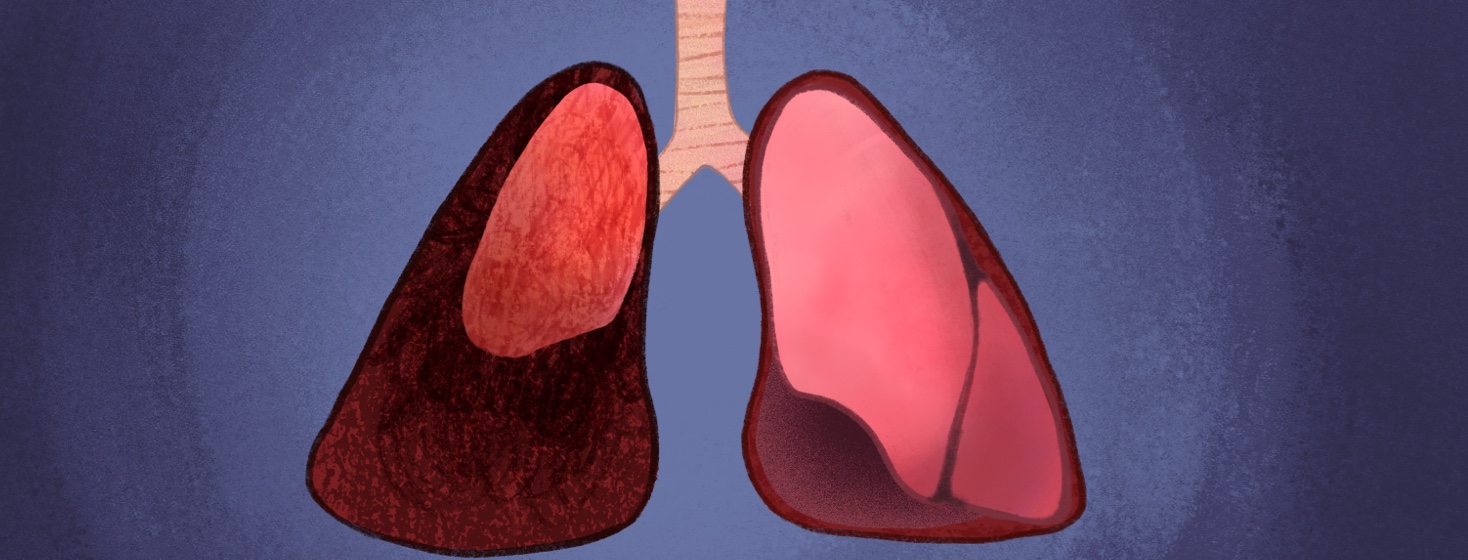
Partial Lung Collapse After Surgery
My college-aged daughter had emergency surgery last month. I knew something was wrong and first took her to urgent care for a diagnosis. A few days later, I then took her to the emergency room (ER) when the pain was unbearable. She needed to see a specialist, but it was a three-month wait, so I took her to the ER for immediate help.
After 6 hours of running tests and trying to figure out what was wrong, the ER doctor finally offered to call the specialist who was already in the hospital.
Yes, please! (What took him so long to offer to page the specialist?!)
Necessary surgery
The specialist said the best course of action would be surgery, and Daughter readily agreed. Why wait another 3 months for a different specialist if this specialist was here and the operating room was available?
Since it had been nearly 8 hours since Daughter had eaten or drank anything, they were able to quickly prep her for emergency surgery.
I called Hubby and told him Daughter was going in for surgery and to hurry to the hospital. He barely made it in time to see her and wish her good luck. He also brought her controller and rescue inhaler, along with charging cords for both of our phones.
It was a quick laparoscopic surgery, and Daughter had an overnight stay in the hospital. I stayed in her hospital room we had several sloooowwwww walks in the hallways to try to prevent blood clots from forming and keep her lungs happy. She has asthma, so surgery tends to make her lungs cranky.
Using an incentive spirometer after surgery
One thing the medical staff uses to help the lungs after surgery is an incentive spirometer.
You may have received one after surgery. It is a handheld device to help keep your lungs strong and inflated. The nurse or respiratory therapist (RT) will usually give you the spirometer and tell you to use it once an hour to prevent a partial lung collapse (atelectasis).
According to Mayo Clinic, "general anesthesia...is a common cause of atelectasis. It changes your regular pattern of breathing and affects the exchange of lung gases. This can cause the air sacs in your lungs to lose air. Nearly everyone who has major surgery has some amount of atelectasis.”1
To prevent that from happening, the medical staff told Daughter to use her incentive spirometer every hour. The spirometer has a small mouthpiece, and she uses that to slowly inhale while trying to get the small ball to hover at a certain place in the tube. Then she repeated that several times in a row.
It is like exercise for the lungs.
Having asthma and a partial lung collapse after surgery
After surgery, Daughter was in a lot of pain and she felt like she could not use the spirometer very often. Then she said she was having problems with her lungs. I noticed she started to cough, was short of breath, and complained that her chest hurt.
The medical staff checked her out and told her she needed to use the spirometer EVERY hour to keep her airways inflated and open. She also needed to keep using her controller inhaler and rescue inhaler (or nebulizer) as needed.
She started using her spirometer every hour, and her lungs gradually improved – as did her surgical sites.
If you have a surgery scheduled and you have asthma, talk to your doctor about using an incentive spirometer or any other treatments they want you to use to keep your lungs happy. Asthma lungs have a habit of getting cranky if anything bothers them.
Has anyone else had a partial lung collapse after surgery? If so, what helped your cranky lungs?
Join the conversation